NIDCR training award supports PhD student’s work revealing new brain circuit for facial pain
Most of us know the aching, pounding misery of headaches. For some people—sufferers of migraines, cluster headaches, or trigeminal neuralgia, which affects the lower face and jaw—pain of the head and face can be debilitating. The burden of these conditions is due in part to the fact that pain of the head and face is measurably different from pain in the rest of the body, both subjectively and in the brain.
Studies have found that people rate head and facial pain as more severe, emotionally draining, and scary than pain elsewhere in the body. Compared to the extremities, pain in the face leads to greater activation of the amygdala, a key fear center of the brain. But beyond that, the underlying neural links between facial pain and emotion have remained poorly understood.
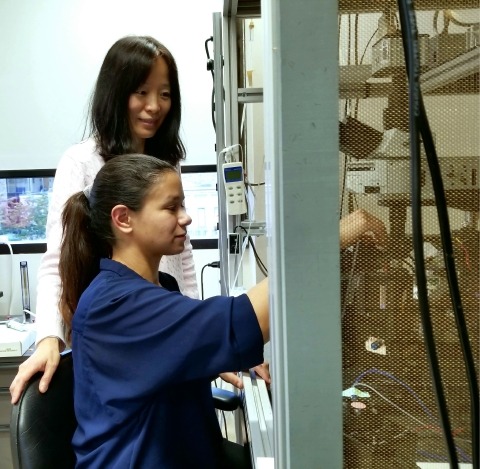
Recently, a group of neurobiology researchers at Duke University led by Fan Wang, PhD, uncovered a potential clue to the heightened emotional aspects of face and head pain. By teasing apart neural pain circuits in mice, the team found a previously undiscovered pathway that conveys facial pain signals directly to a key emotion-related node in the brainstem. The findings, published in Nature Neuroscience, may point to improved treatments for chronic pain conditions affecting the head and face. Much of the research was carried out by Erica Rodriguez, a PhD candidate in Duke University’s neurobiology graduate program. She received NIDCR funding via a Ruth L. Kirschstein Predoctoral Individual National Research Service Award (NRSA) to Promote Diversity in Health-Related Research (F31).
“It Hits Close to Home”
Rodriguez’s own experience with pain inspired her to study pain circuitry in the brain. She still has near-daily pain years after suffering two sports-related herniated discs and undergoing a corrective surgery. “The constant experience of pain, along with the idea of being physically limited, has made me more sensitive to stressful or fearful situations,” she says. “This research hits close to home for me.”
For her research training plan, Rodriguez proposed a series of experiments in mice to delve more deeply into the pain-sensing neurons in an area of the brainstem called the lateral parabrachial nucleus (PBL). It’s an important node along a neural circuit that conveys pain signals between the spinal cord/brainstem and emotional centers higher up in the brain. The pathway is thought to encode the emotional aspects of pain, such as suffering and fear.
Rodriguez’s research training proposal was a success, and in early 2015 she received the award, which provides a monthly stipend, tuition assistance, and support for travel to research conferences.
“Through support for mentored research training and early exposure to the NIH peer-review process, the diversity F31 NRSA is instrumental in jump-starting the careers of promising young scientists,” says Leslie Frieden, PhD, an extramural training officer at NIDCR.
Unraveling Pain’s Pathways
With guidance from Wang, Rodriguez carried out the proposed experiments over the next several years.
Confirming earlier research results, the scientists found that more neurons were active in the PBL of mice after irritating the whisker/facial area than after a similar stimulus to the paw.
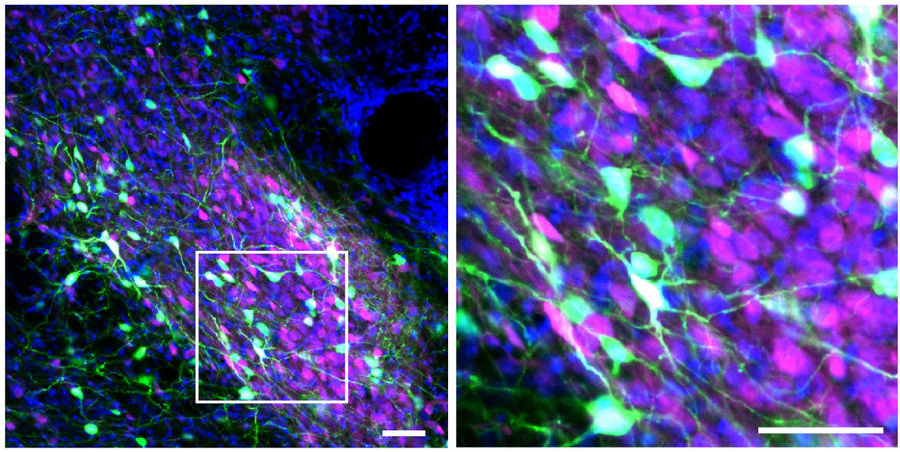
To delve more deeply into why facial irritation caused higher PBL activation, Rodriguez used a novel tool recently developed in Wang’s lab, called "capturing activated neuronal ensembles", or CANE. The technology fluorescently marks specific activated cells, enabling researchers to identify pain-sensing neurons, visualize their connections to other brain areas, and observe their responses to pain signals.
The experiments revealed a previously uncharacterized pathway by which facial pain-sensing neurons are directly connected to the PBL, in addition to the well-defined indirect connections to the PBL by both face and body pain-sensing neurons.
“This new pathway, plus the conventional pathway, is like a double input to the brain,” Wang says. “It appears to explain the heightened response to facial pain.”
To further confirm the findings, the researchers used a technology, called optogenetics, that turns specific groups of neurons on or off with light delivered through optic fibers implanted in the brains of live animals. Activating the newly discovered pathway caused mice to display pronounced behaviors consistent with pain-related discomfort. When the pathway was inactivated, mice became less sensitive to irritation on their faces, but sensitivity to paw irritation remained the same. This result confirmed that the new direct pathway is indeed specific to facial pain.
“This suggests the system is evolutionarily wired to respond to head and face pain more quickly and more intensely,” says Wang.
The results could inform the development of new or improved treatments for chronic pain. For example, a current treatment for chronic facial pain involves surgery to sever the indirect pathway; disrupting the newly discovered direct pathway might improve patient outcomes.
To get this information closer to the clinic, Wang and her colleagues will continue to explore the new pathway, including testing whether its long-term activation contributes to chronic pain conditions of the head and face.
Moving Beyond Pain
With her dissertation work complete, Rodriguez is preparing to graduate in the spring and move to New York, where she will start a postdoctoral fellowship at Columbia University. She credits the NIDCR research training award as an important factor in her success.
“The research, grant-writing, and networking I was able to do with the support of the award helped me develop a skillset that’s prepared me for the next stage of my career,” says Rodriguez. “It boosted my confidence and helped me realize I’m capable of doing science and I’m certain in that ability going forward.”
At Columbia, Rodriguez will continue to study the emotional circuitry of the brain. She hopes that work will eventually enable her to open a lab of her own.
Wang doesn’t doubt Rodriguez will succeed. “Erica is a shining example of why NIH’s efforts to promote diversity are so important,” says Wang. “Talented minority women scientists like Erica will strengthen the scientific workforce of the future.”
In addition to Rodriguez’s NRSA from NIDCR, this work was supported by NIDCR’s Institutional Career Development Award for Enhancing Research Capacity in Temporomandibular Joint Disorders and Orofacial Pain (K12) to Yong Chen, an NIDCR Research Project Grant (R01) to Wolfgang Liedtke, and an NIH Director’s Pioneer Award from the National Institute of Mental Health to Fan Wang.
Reference:
A craniofacial-specific monosynaptic circuit enables heightened affective pain. Rodriguez E, Sakurai K, Xu J, Chen Y, Toda K, Zhao S, Han BX, Ryu D, Yin H, Liedtke W, Wang F. Nat Neurosci. 2017 Dec;20(12):1734-1743. doi: 10.1038/s41593-017-0012-1. Epub 2017 Nov 13. PMID: 29184209.