Series of events restores immune system balance
In healthy individuals, the immune system does a delicate balancing act. It wards off undesirable microbes and viruses and at the same time refrains from attacking the body’s own cells. This restraint is known as immune tolerance.
People with autoimmune diseases such as Sjogren’s syndrome, multiple sclerosis, or type-1 diabetes lose their immune tolerance. As a result, their immune systems destroy organ-specific cells. In the case of Sjogren’s, salivary gland cells are targeted for destruction; in multiple sclerosis, the immune system attacks the fatty sheath that covers nerve cells. In type-1 diabetes, the cells of the pancreas die.
By studying the mechanisms that govern immune tolerance, NIDCR’s Wanjun Chen aims to develop therapies that could block self-destructive immune responses in people who have autoimmune diseases. In a recent paper in EBioMedicine, Chen reported that his lab used a novel immunotherapy to enhance immune tolerance and successfully treat mice that have experimental autoimmune encephalomyelitis, a model disease for multiple sclerosis. The immunotherapy not only eliminated the disease but also prevented disease development in mice.
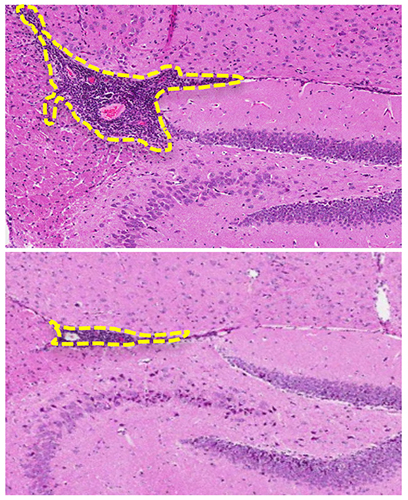
More than 30 years ago, researchers showed that elimination of CD4 T cells (a type of immune cell) prevented and cured the MS-like disease in mice, but the strategy did not work in people who had MS. What Chen’s team did differently was use antibodies to eliminate two kinds of T cells (CD4 and CD8 cells) and give the mice protein pieces (peptides) from nerve cells. One of the specific peptides they used is called myelin-oligodendrocyte glycoprotein, which is important in the formation of the sheath that covers nerves.
The combined steps triggered a cascade of molecular events that were each necessary to a successful outcome. The antibodies caused the T cells to die in an orderly way (a process called apoptosis). The remains of the apoptotic T cells were then eaten by scavenger cells called macrophages. Digestion of the dead T cells stimulated the macrophages to produce a protein called transforming growth factor beta (TGFβ), which drove the generation of regulatory T cells, a category of cells that helps to maintain immune tolerance. Promoting the right kind of regulatory T cells—there are many kinds—was made possible by the immune response of the mice to the nerve peptides used in the treatment.
A novel aspect of Chen’s work is the generation of regulatory T cells that “reprogram” the immune system in mice. Chen is hopeful that optimizing this process may allow clinician researchers to reprogram dysregulated immune responses in humans.
Chen envisions that Sjogren’s syndrome, type-1 diabetes, rheumatoid arthritis, and other autoimmune disorders might one day be treated with variations on this method. “The immune system is broken in all of these diseases,” says Chen. Despite being different in the ways they present themselves, “if you look deeper, there is a common mechanism they share.”
Related Links
Reference
Kasagi S, Wang D, Zhang P, Zanvit P, Chen H, Zhang D, Li J, Che L, Maruyama T, Nakatsukasa H, Wu R, Jin W, Sun L, Chen W. Combination of apoptotic T cell induction and self-peptide administration for therapy of experimental autoimmune encephalomyelitis. EBioMedicine. 2019 Jun;44:50-59. doi: 10.1016/j.ebiom.2019.05.005. Epub 2019 May 13.
Attention Editors:
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research (NIDCR) as the source. We would appreciate if you would also link to the NIDCR website.