Many cancer researchers look for ways to stop the growth of cancer. J. Silvio Gutkind, PhD, is trying a different angle. He aims to piece together the steps needed to build a cancer—specifically head and neck cancer.
“If I can build it, I can understand it,” says Gutkind, a long-time NIDCR intramural researcher now at the University of California, San Diego. He calls this approach reverse engineering. It entails documenting each essential molecular pathway, then determining the precise sequence of events that must occur to turn a normal cell into a cancerous cell. This information could help clinicians tailor treatments to the unique features of each patient’s cancer.
Before Gutkind can build a cancer, though, he needs all the molecular parts—the signaling pathways inside a cell that go awry and send it down a cancerous course. His latest study—a collaborative effort with his NIDCR colleagues and others—maps out a key molecular network in head and neck squamous cell carcinoma. With this study, published in Nature Communications, Gutkind believes his team has found an essential missing puzzle piece.
Traversing a Mutational Landscape
Compared to non-cancerous tissue, tumors are riddled with hundreds or thousands of mutations. These errors scramble molecular networks that govern cell growth, longevity, migration, and more. Over the last decade or so, widespread efforts—such as NIH’s The Cancer Genome Atlas (TCGA)—have mapped these genetic events in dozens of cancer types. Such cancer atlases can help scientists better understand cancer biology and identify potential new treatment targets.
While these troves of genetic data fuel important advances in the cancer field, the wealth of information also poses challenges. For instance: of a tumor’s hundreds of mutations, which ones matter? For a given cancer, just a handful of gene changes—called driver mutations—propel the initial transformation of a normal cell into a cancerous one. Other mutations arise along the way, and they are known as “passenger mutations,” since they don’t seem to play a causative role. To make sense of a cancer’s genetic origin, one must sort the drivers from the passengers.
In the Driver’s Seat
To find the cancer drivers, Gutkind has spent his career identifying and dissecting key signaling pathways that are disrupted in head and neck cancer.
Starting with a 2005 Cancer Research publication, Gutkind and his colleagues at NIDCR and the University of Maryland identified a central pathway in head and neck cancer. Called the mTOR pathway, when its components are mutated or their expression genetically altered, it fuels the uncontrolled growth of cancer cells. The cells grow and divide unchecked, passing their flaws to their offspring. Gutkind’s group found that they could block the dysfunctional mTOR pathway with a drug called rapamycin and thereby shrink head and neck tumors in mice.
Those findings enabled Gutkind and his team to carry out two human trials of drugs targeting the pathway—one in patients newly diagnosed with oral cancer and the other in patients with precancerous oral lesions. Those clinical trials have been completed and the results submitted for publication.
Addressing the Hippo in the Room
The mTOR work, along with studies on other key pathways, has refined researchers’ understanding of the molecular signaling networks that drive head and neck cancer. But, Gutkind says, “we didn’t think these pathways were sufficient to initiate cancer—we were missing something.”
In his search for missing pieces, Gutkind recalled one of his earlier studies in a different cancer, ocular melanoma, the most common cancer affecting the eye. His group found that a key contributor to ocular melanoma was a web of interconnected molecules known collectively as the Hippo pathway. Up to that point, the link between Hippo and cancer drivers was not well-described. Scientists mostly knew about its role in guiding fruit fly development.
“Finding a link between the Hippo pathway and ocular melanoma prompted us to explore whether it was also involved in head and neck cancer,” says Gutkind. Using a mix of bioinformatics analysis, cell culture experiments, and animal studies, Gutkind’s team showed that Hippo, along with two signaling proteins called FAT1 and YAP1, appear to play an important role in the development of head and neck cancer. FAT1 and YAP1 were known to be altered in several cancers, including head and neck cancer, but no one had connected them to each other or FAT1 to Hippo dysregulation in cancer.
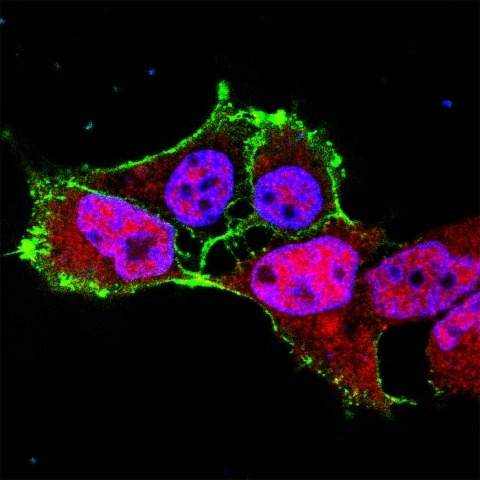
Gutkind’s group showed that in cultured cells under normal conditions, FAT1 acts as a molecular light switch and keeps the Hippo network turned on, which in turn blocks YAP1 from activating cell growth genes. When FAT1 is mutated, as is often the case in head and neck cancer, it fails to activate the Hippo network. This allows YAP1 to turn on cell growth genes, potentially leading to unchecked cell division and proliferation. Gutkind speculates that this network acts as a sensing mechanism that tells a cell to stop dividing when it touches another cell. When the network is disrupted, cells may lose their natural boundary recognition and invade neighboring cells and tissues.
With this information in hand, the scientists tested YAP1’s potential as a therapeutic target. When mice with oral cancer received a drug that blocks YAP1, tumor growth declined and so did cancer cell proliferation. The scientists are continuing to explore the pathway’s potential as a treatment target in humans.
A Builder’s Toolkit
Scientists have now identified major head and neck cancer pathways—networks that guide cell growth, survival, division, damage-repair, and possibly boundary recognition, thanks to the Hippo studies. Gutkind and his team stand ready to put it all together, build a cancer, and find the drivers.
“In about 1 out of 6 people, a precancerous oral lesion will develop into a tumor,” explains Gutkind. “While we know most of the network-disrupting events, we cannot precisely define the order in which they must occur to become cancer. Knowing this might help us identify who is most at risk.”
With NIDCR support, Gutkind and his team are developing an experimental system to address this question. They will use genetic engineering in normal oral stem cells to express different combinations of mutated molecules, hoping to land on the exact formula that will cause the cells to develop cancerous features.
Gutkind says that having a more complete arsenal of information—not just the events, but also the timing—“could help us identify more precise therapies or combinations of therapies to prevent or intercept the process of cancer progression.”
References
Martin D, Degese MS, Vitale-Cross L, Iglesias-Bartolome R, Valera JLC, Wang Z, Feng X, Yeerna H, Vadmal V, Moroishi T, Thorne RF, Zaida M, Siegele B, Cheong SC, Molinolo AA, Samuels Y, Tamayo P, Guan KL, Lippman SM, Lyons JG, Gutkind JS. Assembly and activation of the Hippo signalome by FAT1 tumor suppressor. Nature Communications. 2018;9:2372. doi:10.1038/s41467-018-04590-1.
Feng X, Degese MS, Iglesias-Bartolome R, Vaque JP, Molinolo AA, Rodrigues M, Zaidi MR, Ksander BR, Merlino G, Sodhi A, Chen Q, Gutkind JS. Hippo-independent activation of YAP by the GNAQ uveal melanoma oncogene through a trio-regulated rho GTPase signaling circuitry. Cancer Cell. 2014 Jun 16;25(6):831-45. doi: 10.1016/j.ccr.2014.04.016. Epub 2014 May 29. PMID: 24882515.
Amornphimoltham P, Patel V, Sodhi A, Nikitakis NG, Sauk JJ, Sausville EA, Molinolo AA & Gutkind JS. Mammalian target of rapamycin, a molecular target in squamous cell carcinomas of the head and neck. Cancer Res. November 1 2005 (65) (21) 9953-9961. doi: 10.1158/0008-5472.CAN-05-0921.
NIH Support: This study was supported by NIDCR’s Intramural Research Program and NIDCR grant R01DE026644; the National Human Genome Research Institute; and the National Cancer Institute.