A Coronavirus Sensor that Fits in the Palm of Your Hand
Portable device detects virus within seconds
In Brief:
- In a preliminary study, University of Florida researchers report the development of a hand-held device that rapidly and reliably detects SARS-CoV-2 in artificial saliva.
- The portable sensor could eventually be used for low-cost COVID-19 testing in a variety of locations, including dental and health care settings, schools, the travel industry, and at home.
At the beginning of the COVID-19 pandemic, University of Florida dentist-scientist Josephine Esquivel-Upshaw, DMD, MS, was in one of her weekly meetings with chemical engineering collaborators discussing a dental materials project. One of the engineers mentioned that their group was trying to develop an at-home sensor that could rapidly test for SARS-CoV-2, the virus that causes COVID-19.
In those early days, test samples were usually collected by inserting a long swab deep into the nasal cavity. Esquivel-Upshaw couldn’t imagine that many people would be willing or able to perform this procedure on themselves. There had to be an easier way. As a dentist, Esquivel-Upshaw immediately thought of saliva—evidence that it harbored the virus was just beginning to emerge, and collecting a sample would be as easy as spitting. With her colleagues on board, the team set to work building a testing platform.
Just over a year later, Esquivel-Upshaw and her colleagues now report preliminary results showing that their hand-held sensor can rapidly and reliably detect SARS-CoV-2. The project received NIDCR support as part of the institute’s efforts to provide rapid funding for COVID-19 research early in the pandemic. The non-invasive, re-usable, and portable system is designed for low-cost testing in a variety of locations, such as dental and health care settings, schools, the travel industry, and at home. Although several at-home COVID-19 tests are now sold in drugstores, they rely on shallow nasal swabs and can take up to 30 minutes to display results. By contrast, the Florida group’s device is designed to test saliva and gives results within 30 seconds.
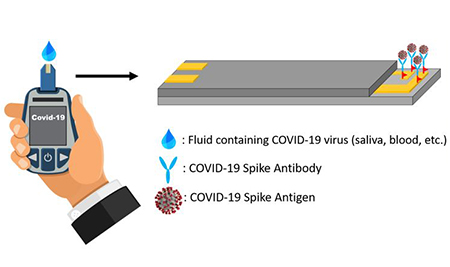
The instrument works much like an over-the-counter blood sugar monitor, where a disposable strip is inserted into a testing device, a drop of blood is applied to the end of the test strip, and a result appears on the device’s screen within seconds.
To customize such a system to detect SARS-CoV-2 in saliva, the Florida team purchased commercially available antibodies that bind, or attach, specifically to the virus, and they developed a series of chemical reactions to affix the antibodies to the test strips. Upon insertion into the sensor, an antibody-laden strip is exposed to electric current generated by an internal circuit board. If saliva applied to the strip contains SARS CoV-2, the viral particles bind to the antibodies, slightly contorting them in the process. These subtle movements create distortions in the electric current—the more virus, the larger the distortions—which are converted into numeric values that appear on the device’s screen.
The scientists tested the sensor’s ability to detect a noninfectious version of SARS-CoV-2, as well as spike protein, which the virus uses to invade cells. Both were suspended in artificial saliva, which was applied to the test strips. The researchers found that the device could reliably detect even very small amounts of the virus or its components.
The next step is to gauge how well the device can detect virus in real saliva from people with confirmed SARS-CoV-2 infection and to compare its performance to gold-standard PCR (polymerase chain reaction) tests. While highly accurate, tests that use PCR require several time-consuming steps that must be done in specially equipped labs, so it can take several days to get results.
Esquivel-Upshaw says the initial outcomes of their comparison studies have been promising. And the sensor’s design means it can be easily adapted to detect other diseases. For instance, Esquivel-Upshaw’s engineering colleagues have used the device to detect the Zika virus and a heart disease-related biomarker. Plans are in the works to adapt the sensor to detect protein markers of oral cancer in saliva. The ability to instantly detect cancer, instead of having to wait days or weeks for results, could mean that patients could start treatment earlier.
“If we can change our detection methods, we can do true point of care,” Esquivel-Upshaw says.
Related Links
- Scientists Find Evidence that Novel Coronavirus Infects the Mouth’s Cells
- NIDCR’s Role in COVID-19 Response
Reference
Fast SARS-CoV-2 virus detection using disposable cartridge strips and a semiconductor-based biosensor platform. J Vac Sci Technol B Nanotechnol Microelectron. 2021 May;39(3):033202. doi: 10.1116/6.0001060. Epub 2021 May 18. PMID: 34055475
Attention Editors
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research as the source.
Subscribe for NIDCR Updates
Receive email updates about the latest advances in dental, oral, and craniofacial research.
October 2024